“All the paths KNEEl before the decisive minds!”
Welcome to this special issue on Knee. Enjoy it with your brew
Redefining the Script: #NeoArmory
Remember when Avengers: Endgame pulled off the ultimate plot twist with the time heist? They didn’t follow the old rules but rewrote them entirely to achieve something bigger. That’s exactly what hit us in today’s Neo-Armory section.
Enter Medacta’s GMK SpheriKA, their groundbreaking take on knee arthroplasty. Like the Avengers’ daring plan to change the past for a better future, the SpheriKA flips the script on traditional knee replacements with its bold kinematic alignment design.
The GMK SpheriKA System
This implant isn’t just an upgrade; it’s a whole new approach.
Medial ball-in-socket stability offers rock-solid support while allowing the lateral compartment to move freely, mimicking natural knee motion.
The funnel-shaped trochlear groove adjusts to various Q-angles, improving patella tracking and minimizing alignment issues.
Designed for Kinematic Alignment (KA), it respects the knee’s unique anatomy instead of forcing it into a generic mechanical alignment.
Performance Check:
Early research shows that KA-based systems like SpheriKA have improved functional outcomes, delivering smoother, more natural movement for patients. The Neo-Armory debate is on: Is the GMK SpheriKA a “heroic move” to redefine knee arthroplasty or just a bold gamble with the status quo? You decide—are we looking at the Endgame of outdated alignment techniques?
Going against the Tide: Meniscus repair #FromTheHistory:
Did you know that for thousands of years—basically from Hippocrates in the 5th century BC up until the 19th century, more than a couple millennia — surgeons believed in sticking to conservative treatment for meniscal tears?
Then came along Sir Thomas Annandale, a Scottish surgeon who changed the game in 1883. Back in those days, they used to call the meniscus the "semilunar cartilage" (sounds fancier, right?). Fun fact: Annandale was already helping his dad in surgeries at the age of 15—impressive, right? Later, he worked with James Syme until 1870 and eventually became a Professor in Edinburgh.
Now let’s talk about the real breakthrough. A 30-year-old miner from North England showed up with sharp knee pain and a joint that would lock up whenever he bent it. Annandale, being the innovator he was, decided to go against the grain. Instead of the usual non-surgical treatment, he tried something revolutionary—repairing the torn "internal semilunar cartilage". He performed an open repair of the torn meniscus with 3 chromic catgut stitches. After immobilizing the knee for seven weeks, the patient fully recovered within six months. Amazing, right? He published this in 1885 explaining the whole operation.
This bold move by Annandale laid the foundation for modern meniscus repair techniques. Thanks to him, repairing meniscus tears is now the gold standard in treatment.
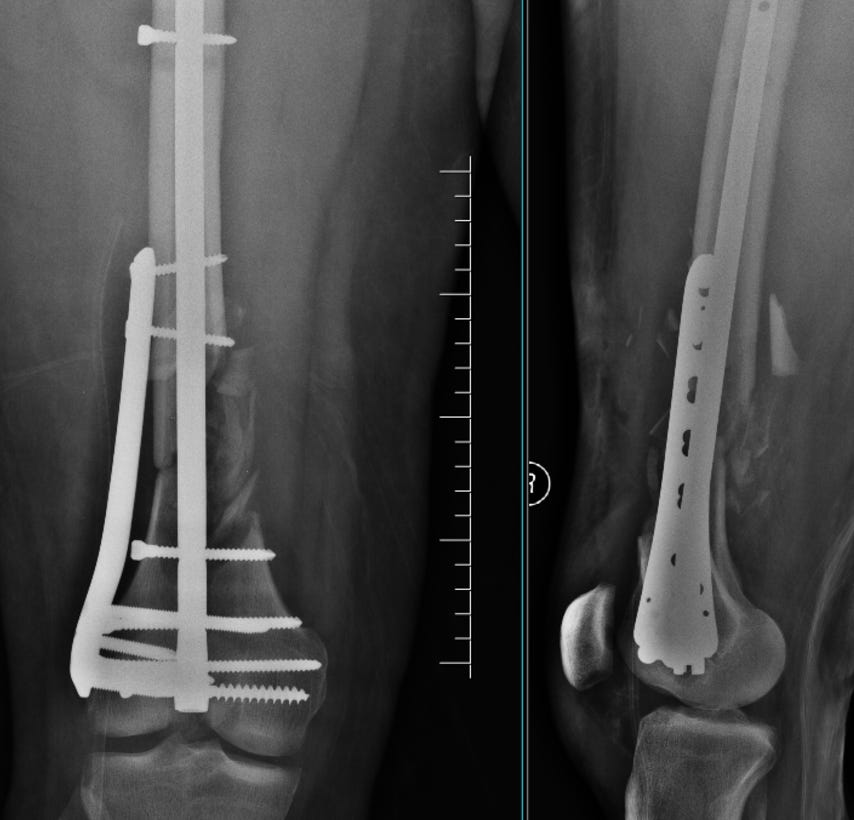
Best of both worlds - The NAIL PLATE construct #SurgicalPearl:
Are you worried about osteoporosis, metaphyseal comminution and obesity when you fix distal femur fractures? - It seems there is a single solution to address all three issues - the nail-plate construct (NPC) combining the retrograde intramedullary nail (rIMN) and locking compression plate (LCP). Both biomechanical and clinical evidence are coming up to support this.
Surgical Technique
1. The affected lower extremity and hip region are freely draped, with the knee placed over a sterile bolster at ~30° flexion.
2. A 3 cm midline incision is made from the inferior pole of the patella to the tibial tubercle.
3. The entry point for the guide wire is confirmed using fluoroscopy. A proximal entry reamer with a retrograde protection sleeve is used, and a long femoral guide wire is inserted.
4. The appropriate length of the retrograde nail is selected to reach the lesser trochanter level for optimal support and splinting.
5. An undersized retrograde nail is inserted into the femoral canal after canal preparation.
6. A separate direct lateral approach is performed to visualize the fracture site if the fracture seems still displaced after nail insertion. Otherwise, a plate of appropriate length is slid through the MIPO technique.
7. The plate’s provisional position is confirmed with fluoroscopy and fixed with K wires
8. The condylar screw (compression bolt) of the retrograde nail is inserted first using the “perfect circle” technique under fluoroscopy, linking the retrograde intramedullary nail (rIMN) and lateral plate. If this is not possible, a condylar screw is inserted and buried into the metaphysis and the plate is placed over it
10. Separate distal interlocking screws are inserted for the rIMN, along with multiple distal locking screws for the lateral plate. Proximal screw holes of the lateral plate are filled with unicortical screws.
11. The rIMN is secured proximally with an anteroposterior screw at the level of the lesser trochanter.
Injectable Blood-Based Biologics for Knee OA: Here’s the Tea 🍵
The ESSKA-ORBIT Group has dropped their verdict on PRP for knee osteoarthritis (OA), cutting through the noise with expert-backed consensus. PRP has legit benefits for knee OA but comes with some dos and don’ts. Let’s break it down:
The Green Flags: PRP’s Winning Moments ✅
• Does it work for knee OA? YES! Clinical evidence supports PRP’s use.
• Severe OA (KL-4)? PRP can still help!
• Patellofemoral OA (PFOA)? PRP is in.
• Post-effusion aspiration inflammatory phase? PRP works here too.
• Repeat treatments? If PRP worked before and symptoms reappear, go for it again.
• Better than hyaluronic acid? Yep. PRP takes the crown. 👑
• Better than corticosteroids? Another yes—PRP has clear advantages.
The Red Flags: No-Go Zones for PRP 🚫
• Asymptomatic early OA? Nope, no rationale for PRP here.
• Disease-modifying effects? Sorry, PRP isn’t magic—it won’t reverse OA.
• NSAIDs, local anesthetics, antibiotics around PRP? Hard no on all three.
• Other injectables like autologous conditioned serum or alpha-2-macroglobulin? There is not enough evidence to support these yet.
The Extras: FYI About PRP 📝
• Best for KL 1-3 OA.
• Contraindications? Infection or cancer.
• Leukocyte-rich or poor PRP? Either works.
• Dosage? 2-4 injections, spaced 1-3 weeks apart.
• Post-steroid timing? Wait at least 6 weeks.
• Patient prep? No high-fat foods or alcohol for 48 hours prior.
PRP is a strong player in knee OA treatment, but knowing when (and how) to use it makes all the difference. Play by the rules for the best results! 💉🦵✨
Another alignment debate #InTrials:
A recent study by Max et al. compared two different techniques for total knee replacement—restricted kinematic alignment (rKA) and mechanical alignment (MA)—using a medial pivot (MP) prosthesis. The results? rKA came out on top, especially for patients with varus knee alignment (where the knees bow slightly inward).
The study, which followed 98 patients with severe knee arthritis for up to two years, found that those who had rKA were more satisfied and had better knee function compared to those who had the traditional MA approach. Scores measuring knee function and how “natural” the knee felt (like the Forgotten Joint Score and Knee Society Score) were significantly better with rKA.
Bottom line? rKA with an MP prosthesis seems to be a game-changer for knee replacements, especially for varus knees. It could mean happier patients, better function, and a quicker return to normal life.
Events to check out:
4th Annual Meeting SIAGASCOT 27th March 2025 Naples, Italy
MIKS 2025 – International Congress on Biological Therapies 3-5 April 2025 Vitoria Gasteiz, Spain
22nd ESSKA Congress 20 – 22 May 2025 Prague, Czech Republic
Answer to last month's question:
Which approach to hemiarthroplasty after femoral neck fractures has minimal complications?
Posterior approach
Direct anterior approach
Direct lateral approach
Anterolateral approach
There is no clinical difference in any of these approaches according to a network meta-analysis by Gusho et al.
Question of the month:
Which nerve block provides effective pain control after TKA?
Continuous adductor canal block
Genicular nerve block
Infiltration between the popliteal artery and capsule
A combination of these
Wait till our next issue for the answer.
Have a fabulous February folks.