Warp speed wrap! #NeoArmory:
“I am Flash” – Flash (DC comics)
We all like speed and precision while operating. Reducing the knife to closure time means bragging rights (also, the patient benefits, etc.. etc). That can happen incrementally by reducing the time taken in each step of the procedure,our and we will employ any device at our disposal.
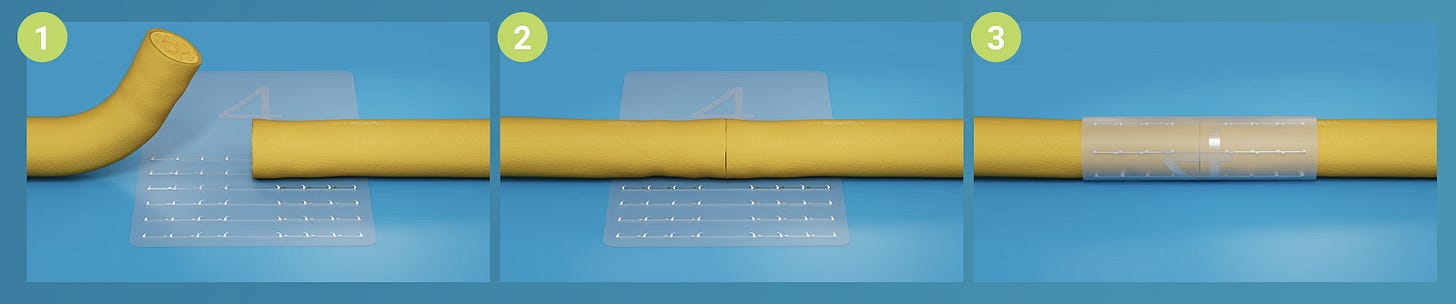
Nerve repairs in complex reconstructions can themselves take upwards of 10 minutes. Biocircuit have devised Nerve tape®, which can cut down this time tremendously. It is a Porcine small intestine submucosal wrap with Nitinol hooks on it. Just get the nerve ends together, wrap the tape around them and move on to the next step.
...and Bob’s your uncle.
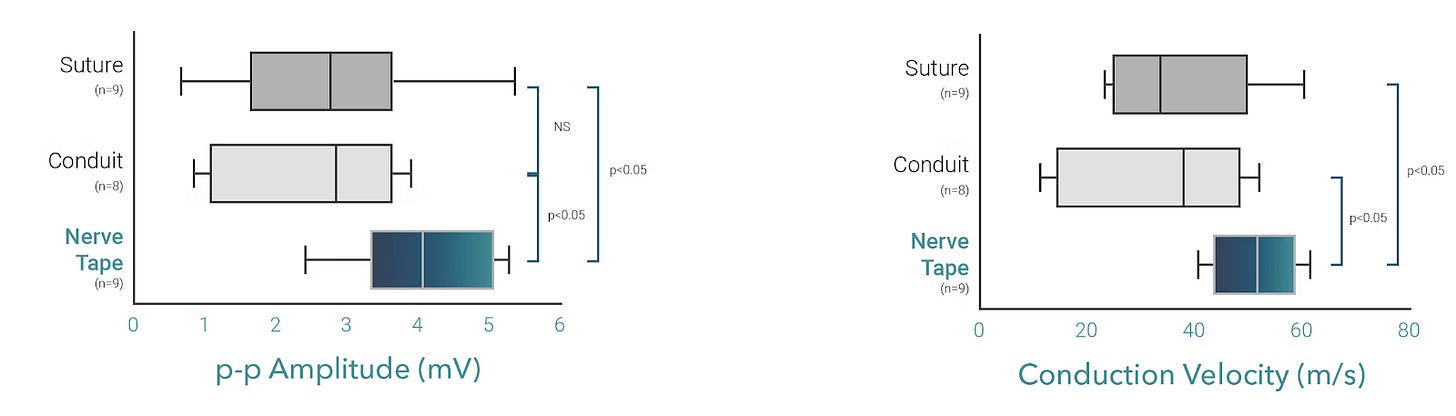
They claim a 97% success rate with repairs, 4.8 times faster and 2.6 times stronger than the microsuture. There is also evidence for better or equal regeneration with data from electrophysiological studies.
This is one of the devices that we expect will become as essential as a skin clip or a bone wax. If you’re not a trauma reconstruction surgeon, get it to your shelf and hope and pray you don’t get to use it.
A psychotic breakdown after Hip surgery –The story of Arthroprosthetic cobaltism #FromTheHistroy:
Dr. Stephen Tower, a hip replacement surgeon from Alaska, USA, an avid cyclist, developed hip arthritis and was finding it difficult day by day. So, he went ahead and underwent Metal on Metal-on-Metal Articular surface replacement (MoM ASR) in 2006, as that was promoted as the one for “highly active individuals. Guess what, he did a 200-mile cycling road race without much difficulty, within 6 weeks of surgery and was on cloud nine as everything seemed great.
Then, after a year and a half, he started feeling these new-onset neurological symptoms like tremors in his hands, ringing in his ears, and he was repeating himself and did not realize he was doing that. Finally, on a fine day, he was supposed to give a talk about Sign nail program that was introduced in Liberia, in Hanford and was staying in a hotel. But now, he went on to have a full-on breakdown and did not leave the hotel room and get this, he wrote on the walls, ceiling, even on the bathroom mirrors with pens, sharpies and when they went out, he even used soap as ink! He was treated by a psychiatrist as bipolar disorder for almost a year and a half.
Tower couldn’t give up on himself and started checking his blood and urine samples and his Cobalt levels were sky high, they were like around 100 times that of known safe blood levels! He called DePuy people (manufacturers of MoM ASR) for no avail and finally, he gave in and went for a revision hip replacement, this time with a Ceramic on poly and unsurprisingly, his symptoms were gone within a month. His surgeon later told him how the prosthesis was virtually a crankcase of metal sludge!
After this, Tower started his research into Cobaltism associated with orthopaedic implants and now an expert in the topic. Can you believe his story was featured in the Netflix documentary “Bleeding edge”.
Cement-Augmented Fixation - a must-know #SurgicalPearl
Here’s a cool surgical tweak that’s making life easier for elderly patients with tricky shoulder fractures. The usual story with locking plates in proximal humerus fractures is that in older bones, the screws can fail, back out, or even poke into the joint—ouch! But in this technique, surgeons added a smart twist: they used shorter locking screws and pumped bone cement through some of them right into the humeral head to improve grip and reduce failures.
The approach is clean and methodical. After a beach-chair setup and a deltopectoral approach, the head and tuberosities are reduced with sutures and wires. Then a PHILOS plate is carefully positioned on the lateral humerus, and screws are placed to engage as much of the humeral head as possible—but here’s the kicker: instead of going long and risking screw penetration, surgeons went short and added cement to the tips of the screws using a special delivery system. Cement was injected through cannulated screws, especially in rows B and D, avoiding rows A (to prevent necrosis) and E (to avoid cement leakage).
What did Foruria et al. find? A dramatic drop in implant failure—from 9% down to just 1%! Patients also showed better function and fewer complications overall. Although a few patients experienced minor issues, such as partial bone necrosis around the cemented screws, the technique appears solid (pun intended). All in all, cement augmentation in the right screws, with the right technique, is proving to be a game-changer for osteoporotic shoulders
Proficiency in Endoscopic Discectomy, when do I reach it? #MostCited:
Given the current trend towards endoscopic discectomy, every spine surgeon aims to master this addition to their spine surgery skillset. However, when is such mastery reached? Li et al. in their work analysed the number of cases needed to bypass the learning curve in percutaneous endoscopic transforaminal discectomy (PETD) and interlaminar unilateral biportal endoscopic discectomy (UBED) in the treatment of lumbar disc herniation. They found that although PETD and UBED surgery are effective in the treatment of LDH with a low incidence of complications, achieving mastery in PETD necessitates a learning curve of 40 cases, while UBED requires a minimum of 15 cases to reach proficiency. So train well to treat well.
A new way to handle the pressure! #InTrials:
Compartment syndrome is a major worry after high-velocity tibial fractures, and while fasciotomy is the go-to treatment, it’s not ideal and comes with risks. This randomised, double-blind study by Jerry et al. explored whether IV Mannitol, a common brain oedema medication, could lower leg compartment pressure and help prevent full-blown compartment syndrome. Forty patients with closed tibial fractures received either 20% Mannitol or saline. Overall, there wasn’t a huge difference in pressure drop between the two groups, but in patients who started with high pressures (≥30 mmHg), Mannitol made a real difference, dropping pressures by about 8.5 mmHg at 1 hour. No side effects were reported. While it’s not ready to replace surgery yet, Mannitol showed early promise, especially for high-risk cases. More studies are needed, but this could pave the way for a simple, low-cost alternative in resource-limited settings.
Events to check out:
IOACON 2025 15 – 20th December 2025 - Guwahati, India
Japan Sports Orthopaedic Association Annual Meeting 12 – 13th Sept 2025 - Tokyo, Japan
18th ICRS World Congress Joint Revolution - 11 – 14th Oct 2025 Boston, USA
Answer to the previous month's question:
What is the standard of care in paediatric ACL injuries?
Early surgical intervention
Delayed Surgery
Conservative Management
Early surgical intervention is better. According to Jin et al’s systematic review of 105 studies on paediatric ACL injuries, Conservative management of ACL injuries in children and adolescents is linked to higher rates of knee instability, secondary meniscal and cartilage damage, and degenerative changes. In contrast, surgical interventions, such as physeal-sparing and transphyseal techniques, yield better outcomes in knee stability and complications reduction.
Question of the month:
Which of the following statements best reflects the evidence regarding the management of elderly patients with femoral neck fractures on clopidogrel?
A) Surgery should be delayed for at least 5 days after stopping clopidogrel to reduce bleeding risk.
B) Early surgery on patients taking clopidogrel significantly increases the need for blood transfusion.
C) Early surgery on patients taking clopidogrel is safe and does not significantly increase bleeding risk.
D) Clopidogrel should always be withheld in the perioperative period to avoid complications.
Wait for our next issue to know the answer
Have a Joyous July folks.





Its me, hi, I’m the team who made this Nerve Tape :)