Good things come in a small package! (At least that’s what she said…) - #NeoArmory:
Gone are the days when Navigation arthroplasty meant lugging around a big machine between theatres on an arthroplasty day. Anything and everything is hand-held nowadays.
Imagine dictating your clinic letters with this Dictaphone… in a ward round… in a trauma bay..
So OrthoAlign, decided why not a handheld navigation device. Their latest iteration is Lantern®, an improvement on their longstanding Kneealign.
Asking the real questions…Can I check Twitter while operating? -
It is an accelerometer-based computer navigation. It is a sensor and small mobile phone sized screen that attaches to their jig and references on the go. Gets your mechanical axis cuts and helps with gap balancing. Chamfer cuts can be done with the implant’s cutting blocks.
The entire set is just one tray of instruments and one disposable. It is implanted agnostic, so it integrates easily into your workflow and multiple cases mean extra sets. The best part is, no need for a pre-op CT. All required software is on the device and no subscriptions. No big consoles and the theatre support staff are going to love it.
This study concludes it can help reduce the malalignment of tibial cuts and avoids breaching IM canals. Interestingly, it reduces tourniquet time.
With ever-advancing kinematic and phenotypic alignment concepts, a device like this can shift us from the ‘art of eye-balling cuts’ to making them patient-specific without huge costs.
Check out this Video
How did OATS begin? #FromTheHistory:
‘‘There are, I believe, no instances in which a lost portion of cartilage has been restored, or a wounded portion repaired, with new and well-formed permanent cartilage, in the human subject.’’ - Sir James Paget
Osteochondral Autograft transplantation and Osteochondral Allograft transplantation have effectively proved the words of Paget wrong and remain cornerstones to manage knee chondral defects. How did these revolutionary procedures come into practice? Well, contrary to popular opinion, allograft transplantation was the first procedure to be tried and tested, years before the development of autograft transplantation.
Erich Lexer in 1908, was the first to try allograft transplantation in human beings. A German surgeon better known for his pioneering works in plastic surgery, Dr Lexer published his experience with joint allotransplantation with three different scenarios - half joint transplantations, both articular surface transplantations and total joint replacements including the joint capsule. His first case was a patient with sarcoma of proximal tibia who underwent proximal tibia transplantation. All transplants were obtained by fresh amputated legs on the same day of surgery. By 1925, Lexer had documented 34 hemi or whole knee allogenic implants in humans and reported a 50% success rate.
With a better understanding of the immunological properties and viability of donor bone and chondrocytes, allograft transplantation has evolved over the years with good success rates. They are now the go-to procedures for large chondral defects. Apart from joint transplantations, Lexer did some pioneering work on the blood supply to bone and understanding of the spread of osteomyelitis.
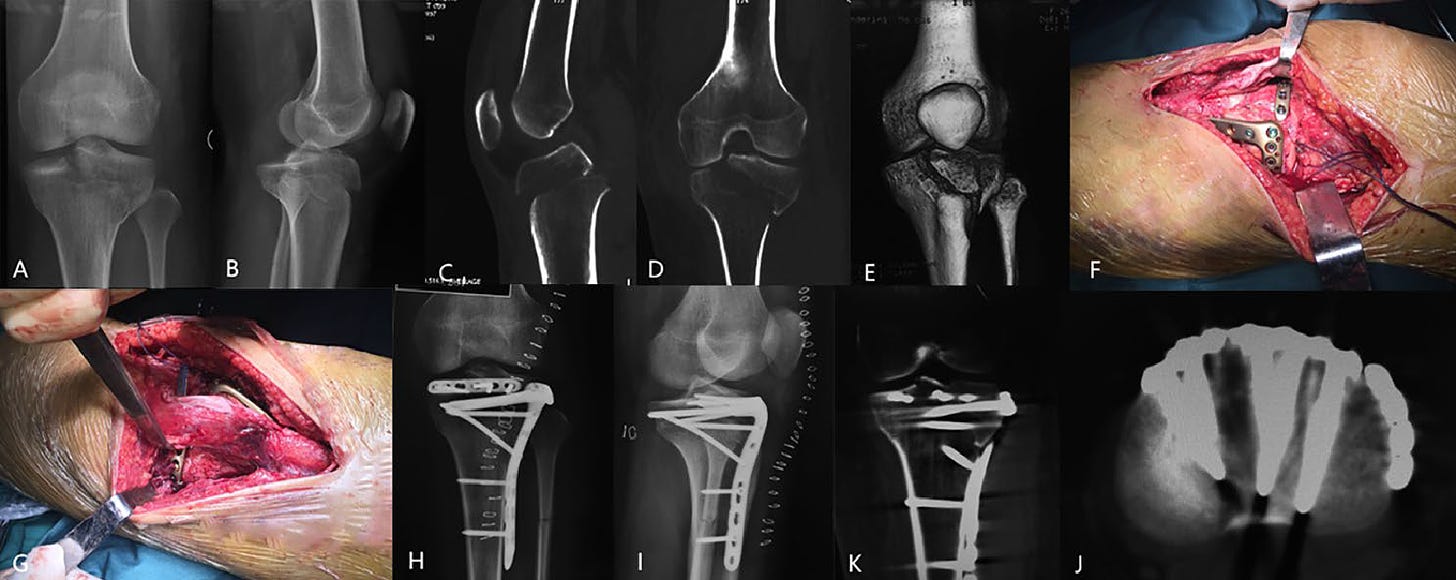
Horizontal rim plates for Hyperextension Knee Injuries: #SurgicalPearl
Hyperextension tibial plateau fractures are always a menace. Anterior depressions are difficult to restore - particularly when they are just behind the patellar tendon where conventional plates can’t reach. Sun et al describe the use of a modified 2.7mm pre-contoured rim plate for buttressing the anterior tibial plateau in hyperextension tibial plateau fractures (HPTF).
Surgical steps:
Approach is standard - medial or lateral plateau - single anteromedial or anterolateral approach. In bicondylar fractures, the initial fixation is performed using combined anteromedial/posteromedial and anterolateral approaches.
Elevate the impaction area of the anterior metaphysis using an osteotome until the posterior slope is restored.
After satisfactory reduction, structural artificial bone augments may be employed if the anterior defect exceeds 1 cm.
For fixing of anteriorly reduced plateau, anteromedial and/or anterolateral locking plates are initially applied.
Further, to reinforce the “bare area” located posterior to the patellar tendon, a 2.7mm plate is pre-contoured to adapt to the curve of the anterior plateau. The plate is inserted behind the patella tendon, proximal to the locking plate.
Screws of appropriate length are then inserted on one or each side of the patella tendon, in a direction parallel to the articular surface- at least one long screw is inserted into the posterior fragment/ uncomminuted medial or lateral fragment to prevent any secondary loss of reduction.
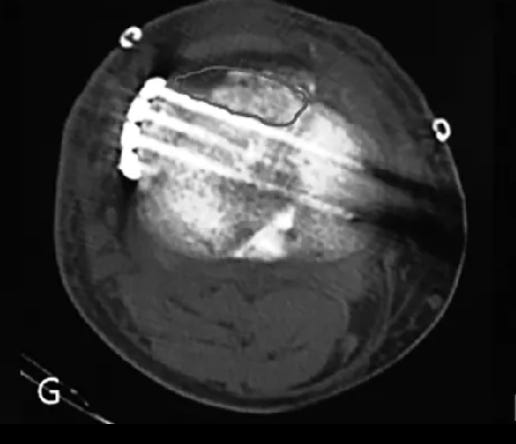
Depiction of the bare area on CT scan
Use of rim plate to address the anterior plateau fragment:
Exercise is better than Drugs in OA!! - #MostCited:
Weng et al. did an interesting network meta-analysis of RCTs comparing exercise to oral NSAIDs and paracetamol for knee and hip OA. A total of 152 RCTs with 17,431 participants were included. For pain relief, there was no difference between exercise and oral NSAIDs and paracetamol at or nearest to 4, 8, and 24 weeks. Similarly, there was no difference between exercise and oral NSAIDs and paracetamol in functional improvement at or nearest to 4, 8, and 24 weeks.
Yeah, NSAIDS can literally be replaced with exercises.
Which is better? Robotics vs Manual Total knee -Results of ROAM Trial: #InTrials:
Robotic TKA (rTKA) vs manual TKA (mTKA) - is the biggest debate going on in the arthroplasty world - a kind of battle between conservatives and liberals
This new evidence is pro rTKA. Clement et al in their RCT of 87 patients, demonstrated superior early knee-specific outcomes in rTKA compared to mTKA. The rTKA group exhibited a more substantial improvement in the WOMAC pain score at two months, with a statistically significant difference.
There is something for liberals too, in the study.
The study revealed no significant difference between the rTKA and mTKA groups in WOMAC functional score at six months. Patient satisfaction, health-related quality of life (measured by EuroQol five-dimension questionnaire utility gain), and fulfilment of patient expectations did not differ significantly between the two groups at the six-month follow-up.
Events to check out:
25th EFORT Congress Hamburg 2024 - 22-24 May 2024 - Hamburg, Germany
The 97th Annual Meeting of the Japanese Orthopaedic Association - 23 -26 May 2024 Fukuoka, Japan
8th Symposium on Current Approaches in Joint Surgery 26 - 29 May 2024 - Bafra, Cyprus
Indian Arthroscopy Society Annual Conference - 12th to 14th September, 2024 - Bangalore, India
Answer for last month's question
What is the ideal way of managing valgus-impacted neck of femur fractures? Is it advisable to conserve them? What are the chances of displacement?
According to a meta-analysis of 47 studies, the displacement rate of 22.8% and 2.8% between the nonoperative and internal fixation groups respectively (p = 0.05). The overall incidence of further operative intervention for each group was 23% and 10% respectively. The cost-utility analysis revealed nonoperative management to be approximately 60% more costly than initial internal fixation when the costs of subsequent surgery were included.
Verdict: Better to intervene valgus impacted femur neck fractures!
Question of the month
When to reconstruct the torn ACLs? What does the current evidence suggest?
Early
Delayed
Does not matter
Hold your curiosity till next month to know the answer. Have a Fab Feb folks…..