First of all, New Year wishes from the Brew with Bones & the Orthopaedic Research Group team folks! We hope you enjoy this year as much as you enjoy our issues. Thank you for your continued support. We have some surprises for all of you in the coming months. Watch this space!
Let’s now dive deep into the hips.
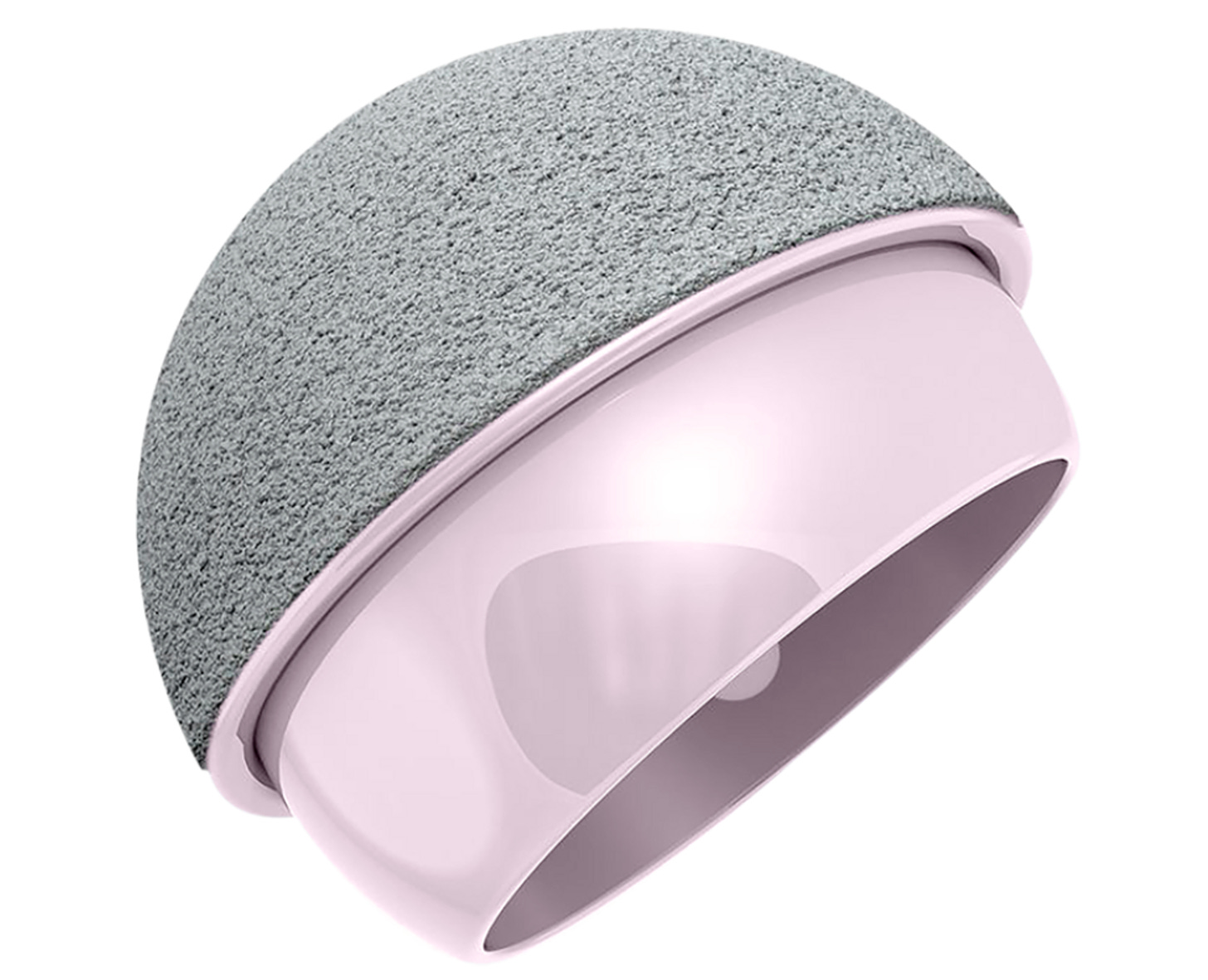
Resurfacing - resurfacing again? - #NeoArmory:
Dear Hip Surgeons, which side of the aisle are you on? Resurfacing or Anti-metal-ions party? There are very few things that polarise a group of people than Hip surgeons’s view on resurfacing.
But MatOrtho brings us an upgrade on the long-used metal-on-metal resurfacing. Meet Recerf®. It is a ceramic-on-ceramic implant with a HA-sprayed shell. Made of Biolox from Ceramtec, the design is based on the long-serving Adept system.
Recerf is currently being used in Canada, Belgium, Australia and South Africa and has more than 400 patients. They have applied for clearance for use in the UK and EU and waiting for clearance for full use by the FDA. They cite navigating a strict regulatory framework as the reason behind their delay.
This is definitely something to keep an eye on but, do note that we don’t have long-term follow-up
The story behind DAA - #FromTheHistory:
In the first year of the orthopaedic internship, Marius Nygaard Smith Peterson assisted in the open reduction of congenital hip dislocation through the Kocher approach. The approach was so bloody that the patient went into shock and survived by a narrow margin. A disciple of Dr Harvey Cushing, his words that one should respect structural planes resonated in Smith Peterson’s mind. He wanted to develop a less bloody approach.
Dr Cushing’s cerebellum exposure, by reflection of muscle flaps with their periosteal attachments, inspired him and gave him the idea of combining the anterior hip approach with the periosteal reflection of muscles from the lateral aspect of the ilium.
He started exploring this possibility in cadavers. He demonstrated the approach to his chief Dr Brackett after ward rounds on a cadaveric specimen. Impressed by the idea, Dr Brackett took the specimen to the American Orthopaedic Association meeting to demonstrate the approach to senior surgeons. Later that year, Smith Peterson started receiving letters from senior surgeons like Dr Fred Albee on the usefulness of the approach in their surgical practice.
That’s how the famous Smith-Peterson approach came into existence folks!
Posterior approach THAs - 90°/45°/0° Stability matters - #InTrials:
Gone are the days, where you have to alarm the patient - “Use a toilet seat raiser, Keep an abduction pillow, limit flexion” & so on after a posterior approach THA to limit chances of dislocation. Intra-operative hip stability at 90° flexion, 45° internal rotation, and 0° adduction is all that matters. Post-operative measures to prevent dislocation DO NOT MATTER.
In a recent RCT, involving 346 patients with an average follow-up of 2.3 years, the group without hip precautions (NP) showed no increase in dislocation rates (0/172 patients, 0%) compared to the hip precaution (HP) control group. Surprisingly, all dislocations (4/174 patients, 2.29%) occurred in the group that adhered to hip precautions, with two cases necessitating revision. The study also examined patient-reported outcomes, revealing no significant differences in mean HOOS Jr. scores at 2, 6, or 12 weeks between the two groups. This secondary outcome reinforces the conclusion that short-term outcomes remain unaffected by the absence of hip precautions.
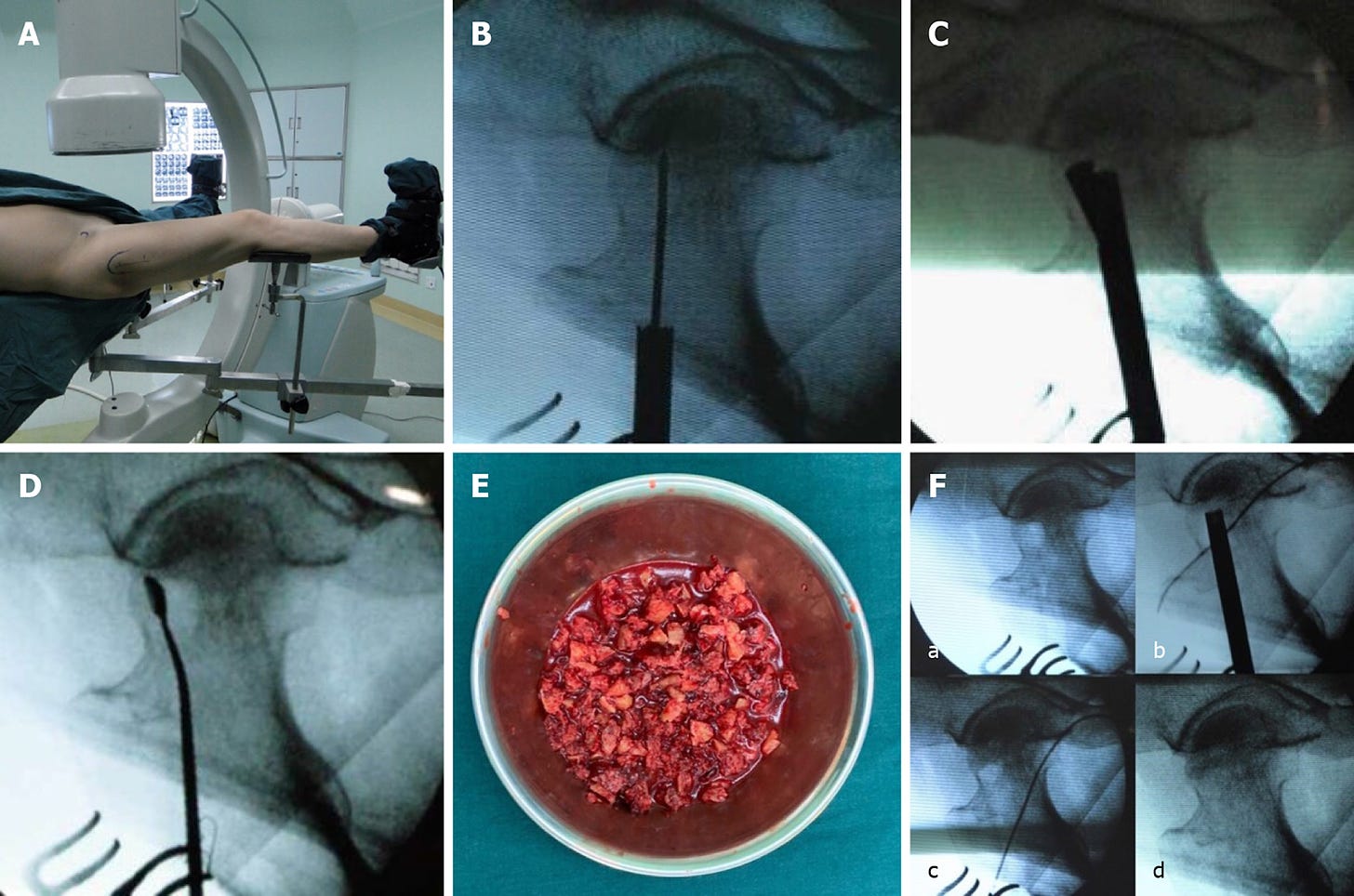
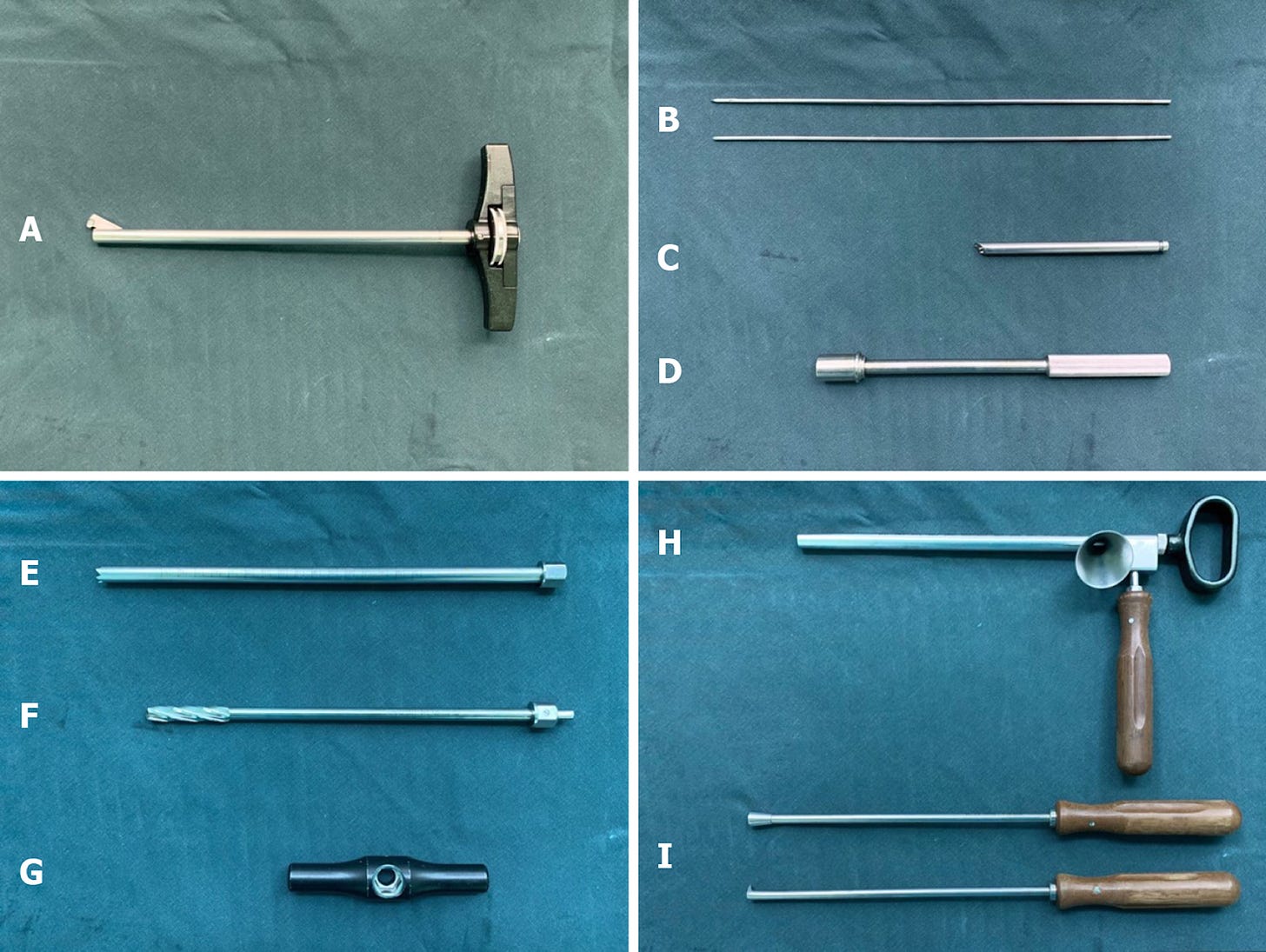
Advanced Core Decompression - #SurgicalPearl:
Advanced core decompression (ACD) involves the use of a single-blade, expandable reamer which helps in better removal of necrotic bone through smaller lateral wall holes when compared to the conventional technique. Now that AVN of the femoral head has become common after COVID, core decompression has also become commoner.
The best point for entrance for the drill is then defined, and a 2-3cm skin incision is made at the distal end of the tuberculum innominatum.
A 2.5mm guide wire is then introduced into the lesion area; following which, the introducer is placed along the guide wire. The introducer is fixed on the lateral femoral cortex.
The introducer is designed such that it enables a safe and easy passage for the trephine through the bone.
A 12mm trephine is then passed into the lesion area under the guidance of the introducer.
The introducer and the guide wire are then removed sequentially.
A 10mm trephine is then passed through the 12mm trephine; and thereby a 10mm core of bone cylinder (consisting of the lateral femoral cortex and cancellous bone of femoral neck) was trephined out.
A single-blade expandable reamer is then introduced into the drilling channel.
By turning the handle and the blade control knob on it, the reamer can be rotated and the blades expanded under image guidance. This enables the resection of necrotic lesions in a precise manner.
A mixture of BMAC and cancellous bone graft then is carefully tamped into the defect using a pestle.
The bone cylinder is finally used to backfill the lateral femoral cortex
The future is probably a Hard Diamond (on hard): #MostCited
Polymeric wear debris causing osteolysis, metal ions causing metallosis and brittle ceramic causing fracture failure - all these force us to search for new bearing surfaces for total hips
Ammarullah et al’s Polycrystalline Diamond (PCD) has the potential to become the next big thing - a hard-on-hard bearing surface. The mechanical properties and biocompatibility are promising.
A computational simulation using a 2D axisymmetric finite element model of hard-on-hard bearing under gait loading has been performed. The percentage of maximum von Mises stress to respective yield strength from PCD-on-PCD is the lowest at 2.47%, with CoCrMo (cobalt chromium molybdenum)-on-CoCrMo at 10.79%, and Al2O3 (aluminium oxide)-on-Al2O3 at 13.49%. This confirms that the use of PCD as a hard-on-hard bearing material is considered the safest option compared to the investigated metal and ceramic hard-on-hard bearings from the mechanical perspective.
Events to check out:
21st ESSKA Congress 2024 08-10 May 2024 Milan, Italy
9th Congress of the Asia Pacific Trauma Society (APTS 2024) 08 -12 May 2024 - Antalya, Turkey
Combined EPOS/POSNA Meeting (2nd EPOSNA) - 08 - 11 May 2024 -Washington DC, USA
Answer to previous month’s question:
How long should Reverse shoulder arthroplasty be delayed after a single corticosteroid injection to the shoulder?
4 weeks
8 weeks
10 weeks
12 weeks
Hold tight till our next issue comes out!’
According to Baksh et al’s all-payer database study involving 1.5 million patients, RSA should be delayed by 4 weeks after steroid injection to avoid the risk of infection.
Question of the month:
What is the ideal way of managing valgus-impacted neck of femur fractures? Is it advisable to conserve them? What are the chances of displacement?
Wait for our next issue to know the answer.
Have a fabulous year ahead folks!