Kids ain't small adults
Let's get updated on the latest developments in Paediatric Orthopaedics, guys!
The Schrödinger’s operation: #NeoArmory:
What do we, Orthopaedic Surgeons, hate the most? Correct! Those pesky ECGs. Second most? Metal removal – Schrödinger’s operation. They are the easiest and the most difficult surgery at the same time. Even more Schrödinger-ery when we must take them off the kids.
Shaheer Maher’s paper (Yep, we completely understood it) shows an alternative method of manufacturing Titanium (Ti) implants with anodization that makes them less susceptible to cell attachment and proliferation.
Invitro testing showed reduced attachment and proliferation of Osteoblasts. They also added Gallium to the mix, and it showed antibacterial properties against S. aureus and P. aeruginosa.
(A very useful photo)
If any of the major manufacturers integrate this into implant manufacturing, that will be great!
The story of Wick Harness #FromTheHistory:
Having been born and studied Medicine in his hometown, Brno, Czechoslovakia, Arnold Pavlik worked under Dr. Bedrick Fejka, also in the same town. Finally, in 1939, Pavlik got “wings” when he was appointed as chief of Orthopaedics in Olomouc, a town around 60 miles away.
Now, now, fate rolled the dice, and his hands were tied as the World War II started and Nazis occupied Czechoslovakia. But, after treating numerous kids with congenital hip dislocations and seeing them end up with Avascular necrosis, he could not sit idle. He started working on a new philosophy, which he called “functional treatment”. To bring it to life, he wanted leather straps, but welcome to the war, he could only find wicks used in petroleum lamps, believe me, that didn’t stop him from glowing. He made a harness which followed his philosophy with those wicks till the war was over, and then got to make with leather. He found that the outcomes with his harness were excellent, with almost negligible incidence of AVN, and he published his findings.
He was being called a forger, and he had to defend himself. Can you imagine that? Having thought out of the box, formulated his principles, made a harness which follows those principles and overall, gives excellent results, only to get hurled insults upon? As refiner’s fire brings out gold, as you know, Pavlik harness with his principles makes the basis of how DDH is treated around the world, even after 3 quarters of a century!
Resurrecting the Lost Art for common upper limb fractures #Clinical Pearl:
Let’s go through the key takeaways from Bryson et al.'s paper regarding the conservative management of distal radius fractures
1. Clavicle Fractures
• Treatment: Broad-arm sling for 10–21 days for pain relief.
• Mobilisation: Begin gentle mobilisation after sling; avoid contact sports for 5 weeks.
2. Proximal Humerus Fractures
• Remodelling potential: High (80% of humeral growth from proximal physis).
• Treatment: Collar and cuff for symptom control for 3 weeks.
• Mobilisation: Start gentle movements at 10 days, full at 3 weeks.
• Exceptions: Only intervene surgically if the epiphysis is rotated >90° and locked.
NB: Full displacement is acceptable if >2 years of growth remain.
3. Supracondylar Humerus Fractures
AO Type I and II:
• Treatment: Collar and cuff in flexion beyond 100°.
• Mobilisation: After 3 weeks.
Type III and IV:
• Treatment: Closed reduction + K-wire fixation.
• Alternative in failed reduction: External fixation or traction (e.g., straight-arm or olecranon screw traction).
NB:
• Posterior angulation can remodel; varus/valgus typically doesn’t.
• Type I/II treated non-operatively unless instability/neurovascular issues.
4. Distal Radius Fractures
Buckle Fractures: Futura splint for 3 weeks; no follow-up required.
Salter-Harris I/II, Metaphyseal, Diaphyseal:
• Treatment: Manipulate in ED using Entonox and diamorphine.
• Plaster: Below-elbow cast.
• Acceptable post-reduction angulations:
• <10 years: ≤20° (metaphyseal/Salter-Harris).
• ≥10 years: ≤10°.
Off-ended Fractures: Manipulation under anaesthesia, plaster; pinning optional.
NB: Avoid manipulation after 10 days (risk of growth arrest); below-elbow cast preferred for function and convenience.
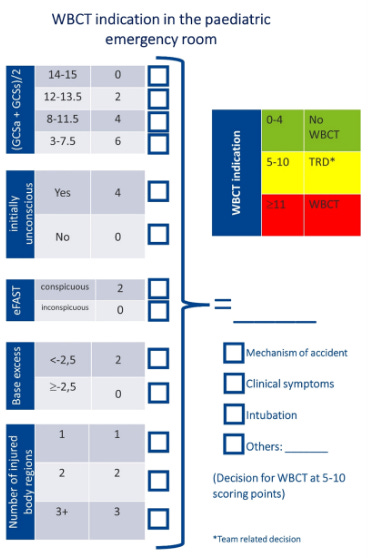
A PePCI for the Injured Child, Please! #MostCited:
Here, PePCI is not the misspelt cola; instead, it’s the newly designed screening tool that necessitates the need for Whole Body CT in injured children, the Paediatric Polytrauma CT-Indication (PePCI) score, as described by Strahl et al. Given the risks of radiation exposure with rampant use of whole body CT, there is a need to rationalise the use of this hazardous investigation, and here it is, PePCI. It considers cGCS, base excess (BE), medically abnormal results from eFAST screening, initial unconsciousness, and injuries involving three or more body regions as significant predictors for a screening tool for decision-making to perform WBCT or selective CT.
Cartoons to the Rescue: Easing Pain and Anxiety in Kids During Pin Removal - #InTrials
Akan et al. aimed to see how much pain and anxiety kids aged 4–12 feel during pin removal after surgery for humeral supracondylar fractures, and whether watching a fun animated video could help. In a randomised controlled trial with 180 kids, four groups were tested: Group 1 had no prep, Group 2 watched an animation before the procedure, Group 3 got ibuprofen (10 mg/kg), and Group 4 got both the animation and the ibuprofen. Pain was measured using the Wong-Baker Scale, Modified CHEOPS, and heart rate; anxiety was assessed using CAM, SAIS, and CEMS. Results showed that watching the animation made a significant difference in lowering pain and anxiety (p < 0.001). Interestingly, animation alone worked just as well as when combined with medication.
Bottom line: A short animated video before pin removal can go a long way in calming kids and reducing pain, making a tough moment just a little easier.
Events to check out:
Japan Sports Orthopaedic Association Annual Meeting 12 – 13th Sept 2025 Tokyo, Japan
AOSSM Annual Meeting 10 – 12th July 2025 Nashville, USA
18th ICRS World Congress Joint Revolution 11 – 14th Oct 2025 Boston, USA
Answer to last month’s question:
Among the following treatments, which is better for conservative management of carpal tunnel syndrome?
Corticosteroid injection
Wrist splint
Placebo injection
All are similar in efficacy
A network meta-analysis by Adindu et al. showed that all the above modalities are similar in efficacy, with corticosteroids doing slightly better in pain control and nerve conduction during the early follow-up.
Question of the month:
Which is the standard of care in paediatric ACL injuries?
Early surgical intervention
Delayed Surgery
Conservative Management
Wait for our July Issue to know the answer. Have a joyous June guys!