A ‘PEEK’ through? #NeoArmory:
Bone Tumours require a Multidisciplinary management coordinated by follow-up imaging. All is well until Orthopods barge in with the pedicle screws and cages. Although MARS-MRI developments have improved imaging, we still have room to make the Radiologist’s life easier. After all, we are the friendly neighbourhood Orthopods.
This is where ‘icotec’ comes in with their BlackArmor® - Carbon-fibre reinforced PEEK pedicle screw and cage systems. Manufactured through their proprietary composite flow moulding and Ti-iT titanium coating, they claim rapid osseointegration, radiolucency, and most importantly allowing Radiotherapy behind it.
KONG®-TL VBR System – Expandable VBR cage appeared to keep surrounding structures well visible in post-op imaging for radiotherapy and planning further treatment.
KONG®-TL VBR System
Where Kong?
Although research shows the safety of CFR-PEEK implants, we are yet to have any high-quality research to see if their radiotherapy to radiotherapy directly impacts outcomes.
Poignant yet Prime - the tale of Dr. Jacob Erdheim - #FromTheHistory:
Jacob Erdheim was born in Vienna to a wealthy Jewish family. Unlike his four brothers, Jacob chose to become a pathologist (Well! pathology chose him). During WWI, antisemitism made it impossible for him to get a job at a university, so he had to settle for a municipal hospital. But guess what? He eventually got promoted to professor of pathology! He went on to probably perform the first-ever autopsy before a motion picture camera, but yeah, it was a silent film.
Jacob was a bit of a recluse, never married, and lived in a room at the hospital. He passed away in 1937, all alone. But before he died, he sent all his pathological materials to Ernest Freund in the USA, hiding them in a rug—probably because of the Viennese Anschluss. That material eventually made its way to Henry Mankin.
Now, why should we care about Jacob Erdheim? Back in the early 20th century, surgeons did their histopathology exams. Erdheim trained C. Howard Hatcher, who then trained four people who would become a big part of the founding members of the Musculoskeletal Tumor Society (MSTS). In the 1950s, surgical pathology became a proper speciality, and surgeons no longer had to write their pathology reports. Can you imagine doing that now? We owe a big thanks to legends like Jacob Erdheim and Howard Hatcher who fathered surgical pathology.
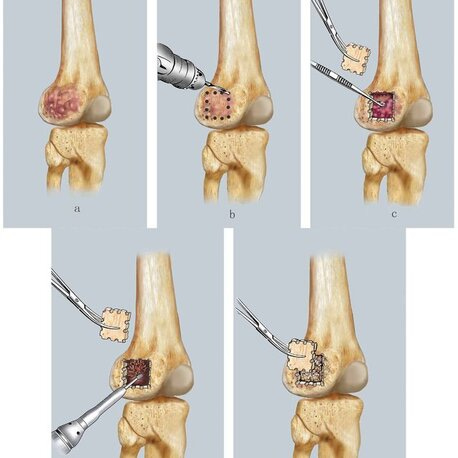
Extending the extended curettage in GCTs - #SurgicalPearl:
The key to successful surgical treatment of the giant cell tumour of bone (GCTB) is extended curettage. There are many methods of doing this with various available adjuvants.
Let us look at the surgical tips for this procedure provided by Manit et al
During exposure, the tissues around the tumour cavity are protected by placing hydrogen peroxide-soaked mops around the tumour cavity.
The soft-tissue mass of the tumour is removed en bloc with a cover of normal tissue to prevent spillage into uninvolved tissues.
Use cautery for this part of the exposure to minimize contamination because high-temperature cautery kills the tumour.
The initial opening into the osseous tumour cavity is made smaller to control the tumour spillage and then enlarged to gain complete visualization.
The walls are curetted, using the sharp edges of the curet.
Tumour cavities often have overhanging osseous ridges with tumours hidden behind them. A curet may not be useful for breaking these hard osseous ridges; a burr is best utilized for this task. In addition to breaking the ridges, a high-speed burr helps to extend the curettage for a few millimetres beyond the grossly visible tumour margin
Adjuvants: hydrogen peroxide is utilized commonly when safe, and argon-plasma cautery is utilized judiciously.
In cases in which >25% of the articular surface is undermined, subchondral bone grafting is recommended before cementing (i.e., a sandwich procedure).
Check out the full text with a video demonstration here
Extending antibiotic cover does not extend the benefits - Complex Endoprosthetic reconstructions- #InTrials:
Check out this recent RCT in JAMA in patients undergoing complex endoprosthetic reconstruction for lower extremity bone tumours. The study investigated whether a 5-day regimen of postoperative, prophylactic intravenous antibiotics could reduce the rate of surgical site infections compared with a 1-day regimen.
604 patients were included in the final analysis. Antibiotic-related complications were significantly higher in the 5-day regimen group at 5.1% (15 patients) compared to 1.6% (5 patients) in the 1-day regimen group. 5 days did not provide additional benefits in preventing surgical site infections compared to a 1-day regimen. Instead, it increases the risk of antibiotic-related complications, particularly Clostridioides difficile-associated colitis.
Keep it short - #antibiotic therapy
Respect Soft-tissues else Recurrent Infections will haunt you! #MostCited
Infection is a devastating complication of endoprosthetic replacement (EPR) in orthopaedic oncology. Infection-free survival following surgical treatment is the dreamland every surgeon wants their patients to be. However, 20-50% don’t find their place there and suffer from recurrent infections.
Azamgarhi et al. analysed the factors responsible for getting recurrent infections following infection of endoprosthetic replacement by considering 133 surgeries done for this scenario. At 2 years follow-up, overall success rates were as follows: two-stage exchange 55.3%, one-stage exchange 45.5%, DAIR with an exchange of modular components 44.6% and DAIR without exchange of modular components 24.7%. Only fifty-one (52%) patients were infection-free at the most recent follow-up. Of the remaining 48 patients, 27 (27%) were on antibiotic suppression and 21 (21%) had undergone amputation. Significant risk factors for recurrent infection were the type of surgical treatment, with debridement alone as the highest risk (HR 4.75); significantly compromised soft tissue status (HR 4.41); and infections due to Enterococcus spp. (HR 7.31).
Verdict: Respect the soft tissue, perform a complete two-stage exchange and pray you don’t encounter Enterococcus if you or your patients don’t want to be haunted by infection again in their lives.
Events to check out:
7th ICRS Summit: From Molecule to Implant: Driving Personalized Knee Preservation Forward 25 – 27 Sept 2024 Catania, Italy
44th SICOT Orthopaedic World Congress Belgrade 2024 25 – 27 Sept 2024 Belgrade, Serbia
56th Congress of the International Society of Paediatric Oncology SIOP 2024 17 – 20 Oct 2024 Honolulu, USA
Answer to last month’s question:
What is the rate of deep infection in case of aseptic revision fracture fixations?
5%
10%
15%
20%
According to Heinz et al, it is 10%.
NB: We are bound to explain this high chance of deep infection every time we revise an aseptic fixation!
Question of the month
Which of the following methods of proximal humerus reconstruction has the lowest 5-year survival rate after tumour excision?
Modular prosthetic reconstruction
Reverse shoulder replacement
Osteoarticular allograft reconstruction
Allograft prosthetic complex reconstruction
Hold your curiosity till our next issue to know the answer!
Have a marvellous month ahead.