WristArt!
‘Sometimes innovation can make us feel that we may have taken a step back. A step back may sometimes be necessary to innovate forward.’ – Anonymous
This quote is not related to our Neo-armory post today. We are just filling out the minimum 200-word limit set by our Editor. Our product in the spotlight today is the winner of ‘Best device named by 10-year-old’ award- WristArt.
WristArt (Guys, seriously.. please reconsider)
Developed by Fibioseq medical Ltd (Acre, Israel), WristArt is a ‘bone sparing’, ‘interim prosthesis’ before the patient undergoes Total wrist arthroplasty. Implant has a double centre of rotation to improve range of motion.
They claim the intramedullary component along with the Extracortical plate helps distribute the forces. It is one-size-fits-all design and non-side specific. Bone preservation allows future revisions easier.
This implant is in very early stages and has had the first human patient implantation. It is a 54 year old with traumatic wrist OA and the follow up shows good ROM. They have just recruited 5 more patients and trial is ongoing. Watch this space for any updates.
PS: Is the quote relevant to this implant now? We’ll let you decide.
A firm handshake that changed the perception of Leprosy #FromTheHistory:
Back around the time India got its independence, Dr. Paul Brand got a call from Dr. Robert Cochrane, the then-principal of Christian Medical College (CMC) in Vellore, Tamil Nadu. Cochrane wanted Brand to join as a teacher. Brand wasn’t too sure at first — he was kind of hesitated, thought about it, and finally said, “Alright, let’s give it a shot for a year.”
Now, Dr. Cochrane was no ordinary guy. He was a well-known dermatologist, especially for his work in leprosy. So, not long after Brand arrived, Cochrane took him on a little field trip — to a leprosy sanatorium near Chennai, about 100 km from Vellore. And that trip? It changed Brand’s life… and ended up transforming the lives of millions of people with leprosy.
Brand wasn’t really into skin diseases — he was more of a “hands guy.” So, he and Cochrane would joke around calling each other the “skin man” and the “bone man.” But their banter led to some serious breakthroughs. During one visit, Brand gave a handshake to a man with leprosy — the man’s hands were badly deformed. Brand asked him to squeeze as hard as he could. And the guy did — so hard that Brand nearly yelled in pain!
That’s when the lightbulb moment happened. Brand realised: the man wasn’t weak… he just couldn’t feel. It wasn’t paralysis — it was loss of sensation, especially pain. Without pain as a warning system, people with leprosy would keep injuring themselves without even realizing it. That insight led to his famous idea — pain, as awful as it feels, is actually a gift. He even wrote a book about it called The Gift of Pain.
Before all this, doctors believed that leprosy caused deformities because of “bad flesh” or flesh-eating bacteria. No one really investigated why the limbs got deformed or how to actually help. But Brand dug in. He researched, experimented, and made huge contributions to hand reconstruction surgery in leprosy patients.
One of his coolest moments? He figured out that the classic “claw hand” in leprosy came from the paralysis of certain hand muscles controlled by the ulnar nerve. He found an old technique by Bunnell (used in war injuries and polio cases) and decided to try it on a young patient named Mr. Krishnamurthy.
Fast-forward a few months and some corrective surgeries later… and boom! One day, Krishnamurthy walked up to Brand, beaming with pride, holding a ball of rice and curry in his hand — something he couldn’t even dream of doing before. It was a small moment, but a giant leap in the world of leprosy treatment.
And to think… all this started with a skeptical visit, a “let’s try it for a year,” and one very, very strong handshake.
Arthroscopic SL lig repair with capsulodesis - #SurgicalPearl:
Want to know a cool way to treat acute and subacute Scapholunate ligament injuries? Know a simple arthroscopic method.
Prone position, wrist in traction, using standard 3-4, 6R, MCU, and MCR portals. Begin with dry arthroscopy to assess the scapholunate ligament (SLL) tear, remove scar tissue, and prepare the scaphoid/lunate for repair.
Use K-wires as joysticks to achieve the precise reduction of the scapholunate interval.
Once aligned, place a 2.2-mm Micro Corkscrew anchor at the dorsal edge of the scaphoid or lunate via the 3-4 portal. Pass sutures through the SLL using a SutureLasso, retrieve them, and secure them with a sliding knot. A second anchor may be added for extra reinforcement.
For dorsal capsular reinforcement, thread a nylon suture through the dorsal capsule, retrieving it via the MCR portal. Shuttle it with sutures from anchor, Knot the sutures securely to reinforce the scapholunate interval while ensuring no tendon impingement.
Final check under arthroscopy to confirm stability and capsular reinforcement. If everything looks good, insert a 1.5-mm K-wire for temporary stabilization and close the portals.
Check the article with beautiful illustrations and original video technique here.
“To Cast or Not to Cast?” – The Wrist Dilemma Gets a Shake-Up!
Ever hurt your wrist, got X-rays, and were told, “It might be a scaphoid fracture, so let’s cast it… just in case”? This study from the Netherlands says — hold up! They looked at 180 adults with wrist pain and totally normal X-rays (the usual “maybe scaphoid” crowd) and split them into two groups: one got the usual 2-week cast, and the other just got a chill 3-day bandage.
What happened? Three months later, both groups had pretty much the same wrist function (measured by QDASH scores). No big differences in pain, grip, or long-term problems. Even better, only 9% actually had a real fracture — and zero nonunions! Bonus points: the bandage group had better wrist movement at 2 weeks and liked their treatment more.
So here’s the twist — if the X-ray is clean, we might be overdoing it with the casts. A bandage and a 2-week recheck might just do the trick. Less fuss, more flex.
Takeaway: Skip the unnecessary cast, save the hassle, and let your wrist breathe — as long as there’s a solid follow-up plan.
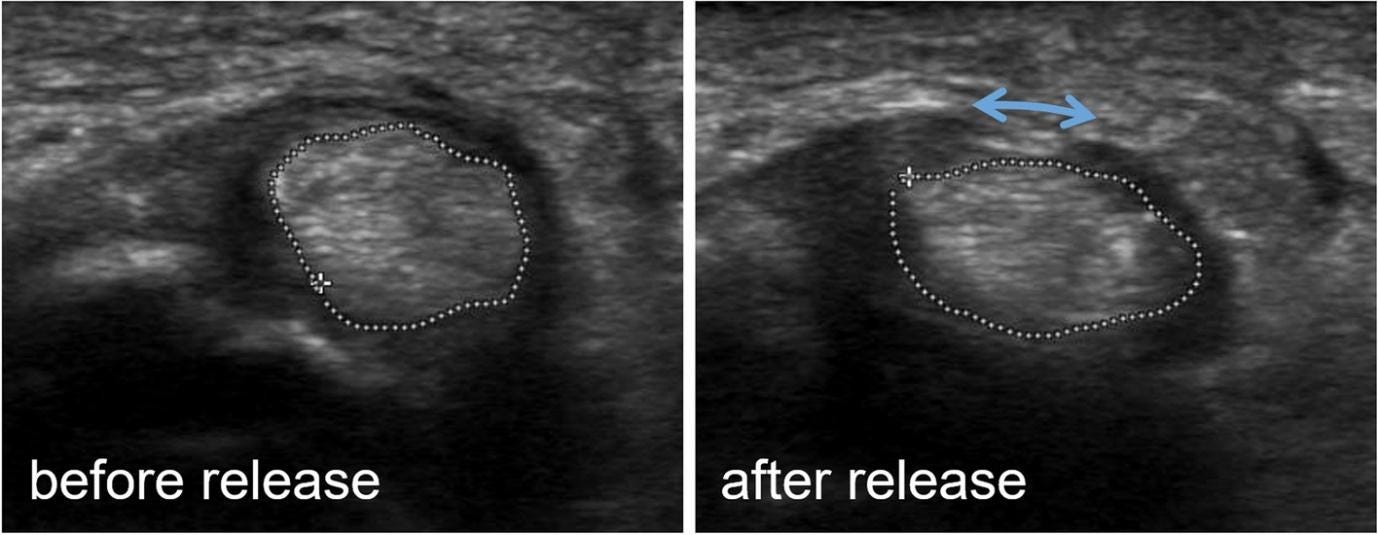
Make the releases even more precise #MostCited:
Trigger finger is a common hand condition that can be treated with percutaneous pulley release. Garcia et al. upon analysis 8 RCTs with 555 patients found that ultrasound-guided release significantly reduced postoperative DASH scores, shortened time to resume activities, hastened discontinuation of oral analgesics, and improved patient satisfaction scores. However, there were no significant differences in VAS scores, time to movement recovery, or surgical success rate.
Events to check out:
Minnesota Anatomic Complex Knee International Symposium (MACKIS) - 28 to 30 May 2025, Eagan, USA
10th Stockholm Arthroscopy and Rehabilitation Conference - 16 to 17 Oct 2025, Stockholm, Sweden
18th ICRS World Congress - 11 to 14 October 2025, Boston, USA
Answer for the previous month question:
Which surgery has low reoperation rate and less complications for patients with glenohumeral osteoarthritis and intact cuff?
A. Total Shoulder Replacement
B. Reverse Shoulder Replacement
Answer: Reverse Shoulder Replacement - according to a meta-analysis of 14 studies by Daher et al.
Question of the month:
Among the following treatments, which is better for conservative maangement of carpal tunnel syndrom?
Corticosteroid injection
Wrist splint
Placebo injection
All are similar in efficacy
Watch this space next month for the answer!
Have a Merry May guys!