Screw the cuff please… #NeoArmory:
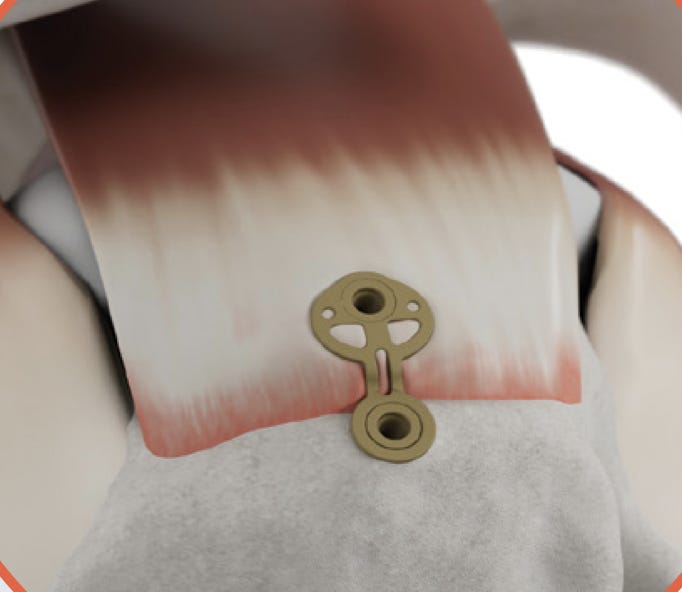
How would a trauma surgeon fix the cuff? They’ll nail it! (ta da). Just kidding... They’ll fix the cuff… with plate… and screw. Nope, not joking this time.
Inovedis, a Minnesota based company have an interesting device that was may be ideated by a trauma surgeon who said ‘Let’s plate the cuff’ (pun intended… ha..haa). SINEFIX is a PEEK based implant designed to be used in rotator cuff ruptures. It has a plate and 2 anchors to hold the cuff tendon in place.
It is supposed to simplify the repair process, minimize post op gap formation and loosening while ensuring blood flow and facilitate healing. This Poster shows, in cadaveric animal testing, Sinefix has higher pull out strength than double row cuff repair. Recently, first patients have had this implanted and watch this space for any updates on those results.
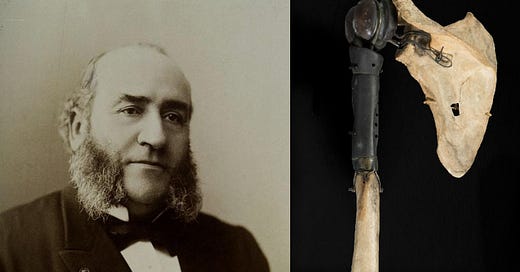
The Surgeon, The Dentist and The Shoulder – That made history! #FromTheHistory:
Back in the early days of germ theory and antisepsis, there was this guy, Jules Pedoux from Paris. He had tuberculosis in his shoulder joint, which led to a nasty abscess. His doctor suggested the usual radical treatment at the time—amputating the whole shoulder! But Pedoux wasn’t on board with that plan.
So, he turned to a surgeon named Jules Émile Péan, who had a wild idea: “What if we just remove the dead, infected part of the bone and replace it with a metal prosthesis?” Sounds futuristic, right? To make this happen, he teamed up with his dentist friend, J. Porter Michaels, to design the prosthesis.
Michaels, being a true craftsman (think Celebrimbor forging the master rings), created the shoulder prosthesis using Vulcanite and Platinum—materials commonly used for dentures since they didn’t rust or irritate tissues. He made it so precise that Pedoux could move his shoulder like normal!
Fast forward to March 11, 1893—Péan went ahead with the first-ever attempt at shoulder arthroplasty! He removed the infected tissue and the humeral head, then implanted the prosthesis. And guess what? It worked! Pedoux even went back to work as a waiter, smoothly opening wine bottles and pouring drinks like nothing ever happened!
Sadly, things took a turn when he developed an infection with multiple sinuses, and the prosthesis had to be removed in 1895. But still, this was a groundbreaking moment in surgical history—Péan’s bold innovation paved the way for modern joint arthroplasty in the early and mid-20th century. And icing on cake, the original prosthesis used by Péan is still up as an exhibit in Smithsonian Museum!
Crazy, right? Who knew a dentist and a surgeon would kickstart the future of joint replacements!
A Three-Step Approach to Brachial Plexus Decompression – #SurgicalPearl:
Neurogenic Thoracic Outlet Syndrome (nTOS) is a pain to diagnose and treat. When the patients don’t respond to conservative treatment, we don’t have a lot of options to try. Arthroscopic decompression of the Brachial Plexus is one surgical option to try
1. Patient Selection – No Shortcuts Here
• Only neurogenic TOS cases qualify. If there’s a cervical rib or vascular involvement, let the thoracic surgeons handle it.
• Start with six months of physio. If symptoms persist or worsen, bring out the scope.
2. The Patient is in a beach chair position, arm in mild traction, and arm in slight flexion/abduction. Anterior, anterolateral, lateral, medial, and trans-trapezial posterior portals are made.
3. Suprascapular Nerve Release – Unlock the First Gate
• Follow the anterior border of the Supraspinatus - Identify the conoid ligament (your lighthouse for the day). Use the outside-in technique to approach the suprascapular notch. Transverse scapular ligament (TSL) = target. Snip it, but watch out for the suprascapular artery hovering above.
4. Step 2: Pectoralis Minor Release – Free the Infraclavicular Space
• Find the coracoid and conjoint tendon. Use radiofrequency ablation to cut the pectoral fascia and release the pectoralis minor. Watch for the musculocutaneous nerve sneaking around.
5. Step 3: Brachial Plexus Release – The Grand Finale
• Locate the costoclavicular space and subclavius muscle. Use RF cautery to clear out fibrous bands strangling the brachial plexus. Be extra cautious with lateral and posterior cords—don’t fry them!
6. Be Ready to Convert - If you hit complications (severe bleeding, nerve injury), switch to open surgery immediately.
#Firstfewcases? Go slow, stay sharp, and have a backup plan. Check out the article and video here.
Active Seniors with Shoulder Fractures - RSA vs Conservative management: #InTrials:
Miquel et al explored whether reverse shoulder arthroplasty (RSA) offers better outcomes than non-surgical treatment for active people over 70 with 3 and 4 part proximal humerus fractures. Eighty-one patients were split into two groups: 41 underwent RSA, while 40 were treated conservatively. After one year, those who had RSA showed noticeably better shoulder function, scoring higher on the Constant-Murley scale (61.2 vs. 52.4). While there were a few complications in the surgical group, including one revision surgery, the overall benefits in mobility and function were clear. The non-surgical group had fewer risks but didn’t recover as much shoulder movement. Overall, RSA stands out as a solid, effective option for older adults who want to stay active —especially when returning to independence is a top priority.
Let’s button up the Latarjet! #MostCited:
Hali et al looked at how two different fixation methods for Latarjet procedure —traditional screws (SF) and newer suture buttons (SB). After analyzing 11 studies with over 1,100 patients, the results were pretty clear: both options work well when it comes to restoring shoulder function, motion, and reducing pain. However, suture buttons had a few perks. They showed fewer complications, especially hardware-related issues, and significantly less bone resorption over time. In terms of strength, both techniques were on par in biomechanical testing. While one study noted a slightly higher rate of redislocation with suture buttons, this didn’t lead to more surgeries. Overall, SB seems like a solid, low-hassle alternative to screws—offering the same stability with potentially fewer problems down the road.
Events to check out
9th Basel Elbow Course 07 – 09 May 2025 - Basel, Switzerland
42nd Annual San Diego Course: Arthroplasty, Arthoscopy and Fractures 11 – 13 June 2025 - Coronado, USA
ISHA 2025 Annual Scientific Meeting 02 – 04 Oct 2025 - Fukuoka, Japan
Answer for the last month question:
What is the best treatment method for syndesmotic ankle injuries?
Dynamic fixation
Static screw fixation
fibular nails
Any of the above
According to a meta-analysis by Cho et al comparing 19 studies dynamic fixation seems to be the superior method of fixation of syndesmosis.
Question of the month:
Which surgery has low reoperation rate and less complications for patients with glenohumeral osteoarthritis and intact cuff?
A. Total Shoulder Replacement
B. Reverse Shoulder Replacement
Wait for our next issue to get an evidence based answer!
Have an amazing April guys.