Barricaid—the band-aid for your spine!
How do we stop something from rupturing back after an operation? “(….lights up a joint…) Just stitch it better bro..” said a dude on the train. “Hmm, ‘stitch it better’, duh… … … Oh yeah! Why not!”
This is how I imagine this was invented
Reherniation after discectomy has been a pain in the back (pun intended) for spine surgeons. We all know the moment we order an MRI on a post-op patient: the monologue that starts when we see a re-herniated disc. Is it the cause of the pain? Do you think I should offer a revision? Going into the previously scarred area is never a nice case to do.
Studies show 44% unsatisfactory outcome and 88% long-term opioid use after revision discectomy. In addition to being less likely to return to work and longer hospital stays.
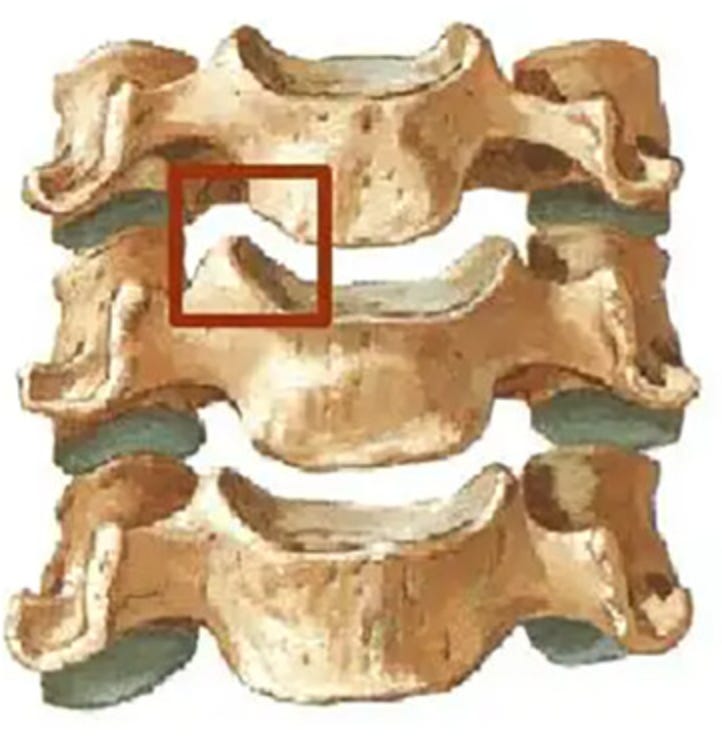
This pain point led to the invention of the Barricaid® ‘only FDA-approved’ device for closing large defects in Annulus.
The metal is titanium alloy to anchor into the vertebral body, and polyester (PET) fabric is used to occlude the annular defect. This can withstand 330 psi of disc pressure while allowing normal anatomical movement.
Inserted under fluoroscopy after discectomy
Studies show that this is superior to discectomy alone. This device significantly reduces re-herniations, reoperations, and re-admissions. This paper shows no difference in revision with or without Barricaid in place.
Going against the wave - the story of spinal fusions: #FromTheHistory:
Russell A. Hibbs kicked off his orthopaedic career at New York Orthopaedic Hospital (NYOH). He made waves in spine surgery from the jump. He was treating cases of Pott’s spine when a wild thought hit him: why stick to old-school splints and braces when you could stabilize the spine from the inside with surgery? Many of his ideas were bold, and didn’t sit well with Chief, Dr. Newton Shaffer—a father figure in American orthopaedics known for playing it safe with non-surgical treatments. But Hibbs wasn’t about to back down.
Hibbs went against the wave, pushed forward with his vision and started seeing serious success. He'd expose the spinous processes, shift them around, and lock them in place to create internal stability. His first-ever patient was a fearless 9-year-old kid. On January 11, 1911, Hibbs went in and fused the boy’s spine from T12 to L3. The kid stayed in bed for a month, then moved on to wearing a brace. Three months later, X-rays showed the fusion had taken hold, and the brace was tossed.
Hibbs kept tweaking his technique, adding moves like mobilizing spinal laminae and prepping the facet joints for better fusion. Over the next 13 years, he teamed up with Risser and Ferguson, performing 427 surgeries and racking up impressive results. The legacy of his work? It's still at the core of how we handle spine deformities today. Hibbs’ hustle changed the game.
Going against waves gave birth to modern-day spinal fusions.
Total uncinectomy #SurgicalPearl:
Total uncinectomy is a reliable method to achieve neural decompression in severe osteophytic foraminal stenosis. This technique will also be useful for cervical osteotomy surgeries for kyphosis. Check out the video technique by Anand et al.
Let us provide you with the pearls.
Smith-Robinson approach to the anterior cervical spine
The lateral elevation of the longus colli is carried just lateral to the uncinate process (UP)
Discectomy is performed and both UPs are delineated.All ventral uncovertebral osteophytes are removed
No.4 Penfield dissector is used to identify the lateral aspect of the UP and protect the Vertebral Artery during the uncinectomy.
Uncinectomy can be performed using a straight osteotome.
The first osteotome cut is directed from cranial to caudal at an anterior
to posterior angle.No bone is removed with this cut; rather it sets the depth of subsequent resection and is safest if it is directed toward the bulk of the vertebral body. For the second cut, the osteotome is passed directly anterior to posterior along the superior endplate. These steps can be repeated 3–4 times progressing posteriorly
Completion of the uncinectomy is confirmed by palpation of the bony boundaries with an angled curette.
PV relieves pain - VERTOS V trial #InTrials:
Is Percutaneous vertebroplasty (PV) really beneficial? A question that lingers in us when we had to convince older patients for the procedure. Let us look at the results of a trial by Carli et al comparing PV with anaesthetic infiltration in chronic osteoporotic vertebral compression fractures (OVCFs). There were 40 participants in each group with a mean age of 69 and 71 years.
At 12 months, the PV group showed greater pain reduction (VAS difference of 1.3 points) and better quality of life improvement than the control group. Analgesic consumption was reduced. There was no significant difference in disability improvement.
Verdict: PV relieves pain but does not improve the disability
Diabetes - ?mother of all culprits - #MostCited:
A major cause of lower back pain is IVDD i.e., intervertebral disc degeneration. Like in most cases (at least as we conclude) aetiology and pathophysiology of IVDD are not yet completely clear. Mechanical reasons were proposed to contribute to the pathology.
Guo et al. in their bidirectional mendelian randomization study using genome-wide association studies with a sample size between 54,358 – 766,345 patients found that metabolic disturbances appear to have a more significant effect on IVDD than biomechanical alterations. Individuals with type 2 diabetes, elevated triglycerides, fasting glucose, and elevated HbA1c are at higher risk for IVDD. Hence, IVDD seems to be preventable by controlling these modifiable risk factors identified.
Events to check out:
Global Spine Congress 2025 28-31 May 2025
Rio de Janerio, Brazil
22nd ESSKA Congress 20-22 May 2025
Prague, Czech Republic
Orthopaedic Research Society 2025 Annual Meeting7 - 11 February 2025
Phoenix Arizona, USA
Answer for the September month’s question:
The popular choice was right - Most resolve spontaneously according to a meta-analysis of 599 patients.
Question of the month:
Hold your curiosity till our next issue. Have a fabulous month ahead guys.